 LEXINGTON, Ky. — Cancer treatment providers can and should do much more to help patients stop smoking. University of Kentucky Markey Cancer Center experts Timothy Mullet, M.D., and Jessica Burris, Ph.D., are co-authors of a recent study that reveals critical gaps in how oncology programs assess and address smoking cessation for their patients.
LEXINGTON, Ky. — Cancer treatment providers can and should do much more to help patients stop smoking. University of Kentucky Markey Cancer Center experts Timothy Mullet, M.D., and Jessica Burris, Ph.D., are co-authors of a recent study that reveals critical gaps in how oncology programs assess and address smoking cessation for their patients.
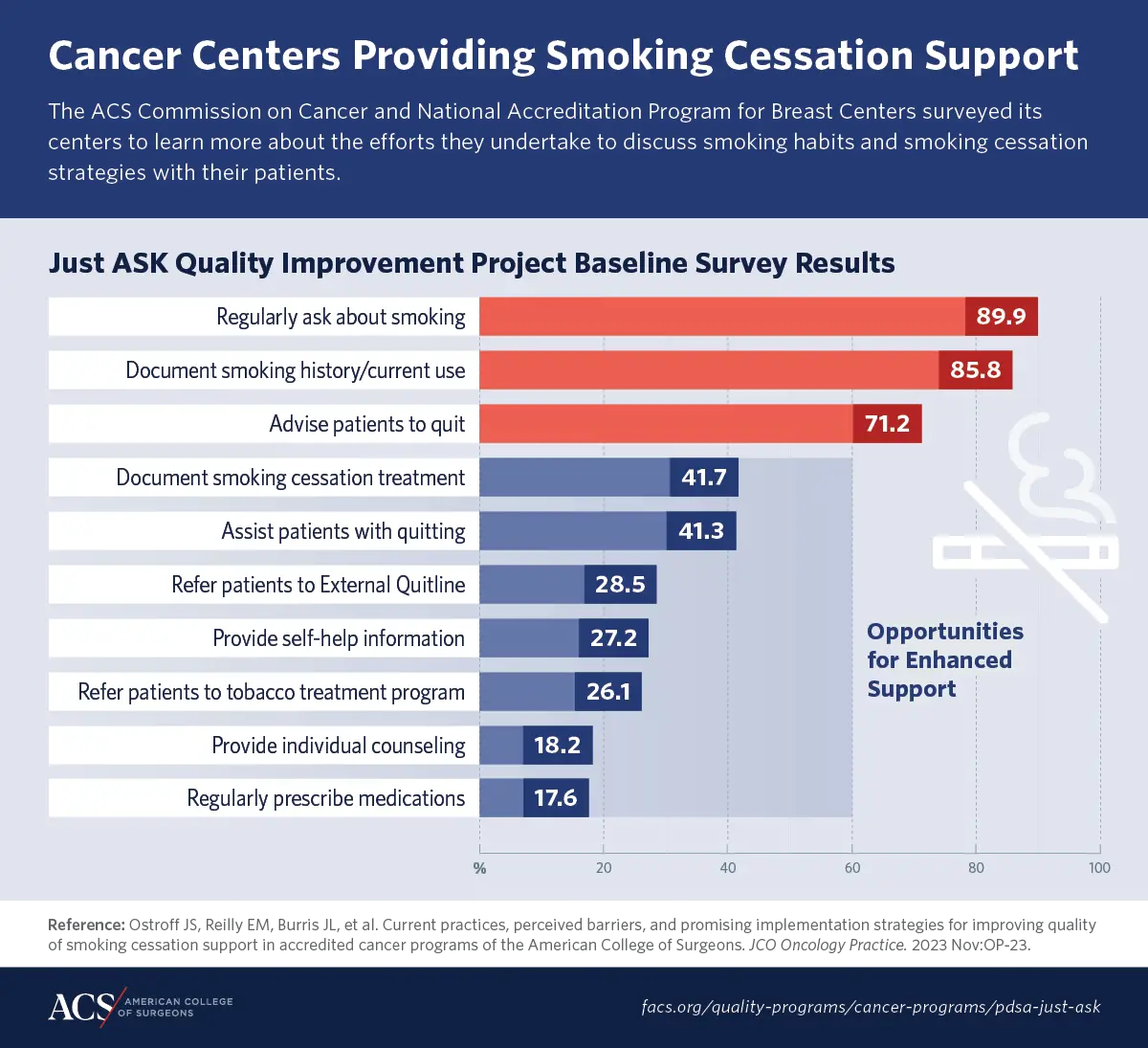
The study published in JCO Oncology Practice highlights baseline survey results of the “Just Ask” national quality improvement project led by the American College of Surgeons (ACS) to improve smoking cessation support in cancer care.
The results represent one of the largest national surveys examining the quality of tobacco treatment in cancer care in a wide range of clinical oncology settings, including academic facilities and community cancer programs.
Smoking among patients diagnosed with cancer is associated with treatment-related complications including cancer recurrence, poor survival, and increased treatment costs. Despite these risk factors, nearly 25% of new patients with cancer and 16% of cancer survivors report current smoking. Many more patients report wanting to quit, but fewer than 10% are successful.
The survey of 776 programs found significant differences in how they assess and treat smoking. While most reported routinely asking patients about their smoking status, less than half documented a treatment plan or helped with quitting.
“While many people understand the role of tobacco in terms of causing cancer, they may not understand the impact that tobacco use has when patients are being treated for cancer,” said Mullett, chair of the ACS Commission on Cancer (CoC) and UK Markey Cancer Center surgeon. “Additionally, many providers may not think about tobacco cessation in terms of treatment. But just like there are effective treatments for high blood pressure or thyroid disease, there are effective treatments for tobacco use. That’s the disconnect we’re trying to highlight in this study.”
The authors outline several practical recommendations to improve the quality of tobacco treatment for patients with cancer and acknowledge that more research is needed to evaluate the implementation of these strategies. A second quality improvement project called Beyond Ask will address building programs’ capacity to offer cessation assistance.
Incorporating Evidence-Based Tobacco Treatment in Cancer Care
The authors outline several recommendations to improve the quality of tobacco treatment for patients with cancer, including:
- Have a proactive system in place for screening patients about their current smoking status.
- Provide greater attention to staff training to help centers adopt best practices for tobacco treatment throughout diverse cancer care settings.
- Establish learning collaboratives or communities to accelerate the implementation of clinical practice guidelines for tobacco treatment and tailor these initiatives to local settings.
- Identify and provide local referrals and other community resources to advise patients about smoking cessation.
More research is needed to evaluate implementation strategies aimed at improving evidence-based tobacco treatment in diverse cancer care settings, the authors said. A second QI project led by the CoC, called Beyond Ask, is focused on building programs’ capacity to offer cessation assistance to newly diagnosed cancer patients who report currently smoking. Results of that QI project are forthcoming.
Highlights from the study and more about the projects can be found here.



















